OSCE Prep: Pediatric Breath-Holding Stations
This guide provides a comprehensive overview of breath-holding spells, addressing both OSCE and theoretical aspects in pediatrics exams. It starts by outlining the OSCE station and then delves into various aspects of the theoretical part which are extremely important while attempting both OSCE and Theory questions.
The following theory and OSCE questions were asked in previous exams.
- Treatment of Breath Holding spells June 97 Marks -10
- Breath Holding spells. June 98 Marks-15
- Breath Holding Spells. June 2017 Marks-4
- Breath-holding spells. Dec 2020 marks 5
OSCE Station Title: Breath-Holding Spell
Scenario: You are the pediatrician on call in the emergency department. A 2-year-old child has been brought in by their parents due to episodes of breath-holding spells. The parents report that these episodes have been occurring for the past few months. The child has experienced two episodes in the last week, each lasting for about 20 seconds. The parents are concerned and seeking advice.
The task to be completed :
Following is the outline of tasks that have to be performed, individual tasks are discussed in detail subsequently.
- History Taking: Obtain a focused history from the parents. Inquire about the onset, duration, triggers, and characteristics of the breath-holding spells. Read the classical chain of events in the clinical feature section below. Ask about any associated symptoms, such as changes in color or consciousness during the episodes.
- Physical Examination: Perform a thorough physical examination of the child. Pay attention to neurological and cardiovascular examinations. Look for any signs of trauma or underlying medical conditions. Details here
- Parental Education: After gathering information, explain to the parents what breath-holding spells are, their common triggers, and the benign nature of most cases. Discuss any potential concerns and reassure them about the child's overall health. Details Here
- Next Steps: Outline a plan for further evaluation or management, if necessary. Discuss when a follow-up visit might be required and what signs or symptoms should prompt immediate medical attention.
- Invite questions
The commonly asked question by the dummy parents in OSCE station could be
How can I help to prevent further breath-holding spells in my child?
A typical answer could be,
Helping your child to learn to deal with frustration, fear, and anger may help. Encourage them to use their words when they are beginning to get angry or frustrated and try to ensure they aren’t overtired. We can offer a session with a professional (psychologist, development physician) for more advice on helping you and your child deal with fear.
Is my child holding his breath on purpose to get things the way he/she wants?
A typical answer could be,
It is unlikely your child is holding his breath on purpose, even if it looks like he’s holding his breath as part of a tantrum. Some children, however, may hold their breath to get what they want during a tantrum if it has proved a successful way to get what they want in the past.
Is there any treatment or prevention available?
A typical answer could be,
BHS doesn't need any treatment as such, Explain how to avoid triggers as explained in the treatment section below. Iron deficiency anemia is more common in children who breathe hold. We will check the child's iron levels and may start an iron supplement to try and reduce the frequency of spells.
Assessment Criteria in the OSCE exam:
| Ability to establish rapport with parents and child. |
| Appropriateness of questions asked during history taking. |
| Thoroughness and accuracy of the physical examination. |
| Clarity and effectiveness of communication with parents. Encouraging asking questions and answering them |
| Good understanding of breath-holding spells and appropriate management. |
Time Allotted: 7-10 minutes
The following part of the post covers all the theoretical aspects of Breath-holding spells
Introduction
Breath-holding spells (BHS) are the most common Nonpileptic paroxysmal disorders in infancy. Since they can be confused with epileptic disorders and syncope, it is important to differentiate them. Also, since most of these cases, just need reassurance to parents, it is even more important to make this distinction.
It is a reflex and not an on-propose act!
Age group
Commonly seen in children of age ranging from 6 mo to 6 years. However, they are reported in children as young as 20 days. Read Breath Holding Spells in a Very Young Infant [External link]
The age at onset is as follows
| Age | Occurrence |
| Neonates | 5% |
| First 6 months | 12% |
| First Year | 66% |
| First 2 years | 94% |
Note - Almost all the children who may develop breath-holding spell will manifest by the age of 2 years
What are breath-holding spells?
Breath-holding spells classically involve the following sequence.
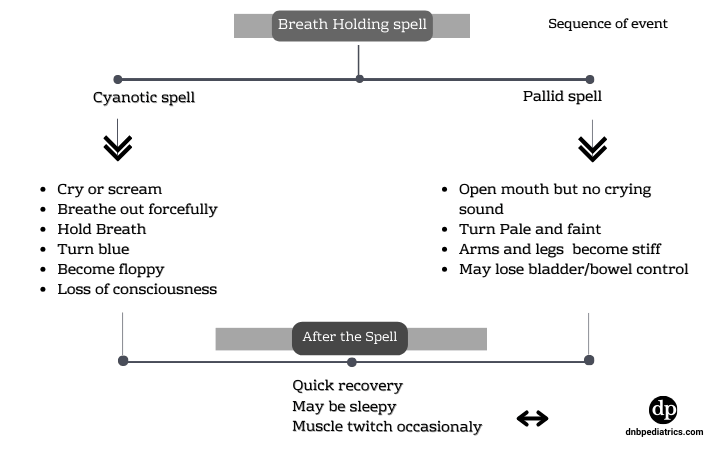
Precipitating factors such as anger or crying result in the involuntary holding of breath followed by cyanosis, loss of tone, transient unconsciousness, and occasionally a brief hypoxic seizure. This is always followed by full recovery within 1 minute.
Triggers for breath-holding spells?
- Anger
- Frustration
- Pain
- Bouts of cry
- Fear, sight of blood, sudden stress
- Dehydration, heat, hot showers
- Standing for a long time without movement
Cyanotic Breath-holding spells are usually precipitated by anger or frustration while pallid spells are more often precipitated by vasovagal mechanism due to pain, fear, heat, etc
Types of BHS

Etiopathogenesis

Anemia and breath-holding spells
It is postulated that children with anemia are more irritable than children with normal hemoglobin levels and are thus prone to a greater incidence of BHS. They have a lesser oxygen-carrying capacity and increased oxygen consumption which increases even more due to triggers. This may contribute to the anoxia causing more severe and longer spells.
Clinical features
The typical sequence of events is
Provocative stimulus
↓Apnoea/bradycardia
↓Color change/cyanosis
↓Limpness/loss of tone
↓Posturing/brief seizure
↓Full recovery from the events, sometimes followed by sleepiness, tiredness
Diagnosis
The diagnosis of the breath-holding spell is typically clinical and the presence of classical sequence usually confirms the diagnosis.
- A. Detailed and focused history-taking is the key. This should include a descriptive summary of the chain of events (as described in clinical features), duration of the event, and recovery. and a video recording if possible.
- B. Complete physical examination including growth and development, neurological examination, red flag signs, and cardiovascular examination including rhythm disturbances.
- C. Imaging - Neuro-imaging is not required unless any abnormal findings are present.
- D. Labs - No particular blood tests are required except Hb levels since Anemia is known to be associated with BHS and correction of anemia is seen to be associated with the resolution of BHS.
Treatment Approaches
A. Parental Education
- Emphasize the benign nature of most BHS to alleviate parental anxiety.
- Provide guidance on recognizing triggers and implementing preventive measures.
- Offer Basic CPR training.
- Offer professional psychological help, if extremely anxious on case to case basis
B. Reassurance and Support
- Offer reassurance to parents, emphasizing that BHS does not cause long-term harm.
- Encourage open communication, addressing parental concerns and questions.
C. Identification and Management of Triggers
- Discuss with parents to identify potential triggers (e.g., frustration, pain) and develop strategies to minimize these triggers.
- Behavioral interventions, such as teaching parents how to respond calmly during episodes, can be beneficial.
D. Iron Supplementation
Some studies suggest a correlation between BHS and iron deficiency. Consider evaluating and supplementing iron levels in affected children.
Some recommend iron therapy at 5mg/kg/day for up to 16 weeks may reduce the frequency and duration of BHS (Cochrane Review 2010)
E. Pharmacological Interventions
- While no specific medication is universally recommended for BHS, some studies propose the use of atropine or oral glycopyrrolate in severe cases.
- Some studies suggest the use of Piracetam is safe and effective in severe cases of BHS
Individualize medication decisions based on the severity and frequency of episodes. - Antiepileptic drug therapy has no role in the treatment of breath-holding spells.
F. Follow-Up and Monitoring
- Follow-up Visits are crucial to assess the child's progress and make any necessary adjustments to the management plan.
- Monitor developmental milestones, iron levels, and the frequency and severity of BHS.
G. Care at home during the episodes
- Parents should be advised to lay down children on their sides while ensuring the safety of their surroundings.
- They should remove objects from around your child to prevent injury.
- During the episode, nothing should be placed in their mouth, including fingers.
Author

Ajay Agade | DNB(Pediatrics), FNB(Pediatric Intensive Care), Fellowship in Pediatric pulmonology and LTV
Ajay is a Paediatric Intensivist, currently working in Pediatric Pulmonology & LTV at Great Ormond Street Hospital NHS, London
Author

Vasu Burli | DNB (Pediatrics), Fellowship in Pediatric Critical Care
Vasu completed his Pediatrics residency at Kanchi KamaKoti Childs Trust Hospital, Chennai and received further training in Pediatric Intensive care in India and UK
💡 Join the Discussion!
🩺 Help us refine this article — share corrections or additional information below. Let's elevate the accuracy of knowledge together! 💉💬